Simulating an interventional platform concept at SSM Health Saint Louis University Hospital
SSM Health utilizes SIMUL8 to make planning decisions for its campus renewal project in less than three months.
In 2015, Saint Louis University Hospital was acquired by SSM Health System under an agreement that a new hospital facility would be developed within a five-year time frame, starting in 2017.
Frank Zilm, Chester Dean Director of the Institute for Health and Wellness Design, was selected along with four other leading firms to drive the planning phase of Saint Louis University Hospital’s $550 million renewal project.
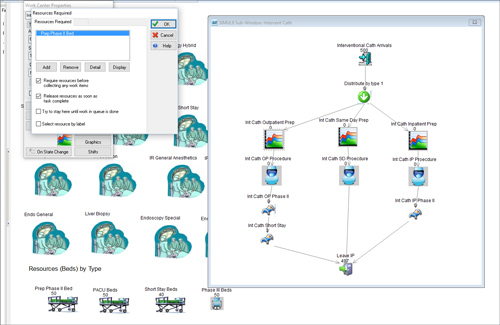
The team recommended the use of an interventional platform, integrating surgery, cardiac, interventional radiology, and endoscopy services, to achieve a more efficient and flexible healthcare campus that will be capable of coping with future demands.
Although this new facility offered SSM Health an opportunity to revolutionize the way that future healthcare services are delivered, it was crucial that any operational and organizational changes could be fully evaluated to ensure physician and staff confidence in the plans.
With less than three months available to complete the planning and programming of the entire complex, SIMUL8’s simulation software enabled rapid and thorough testing of the interventional platform.
"The challenge that we had was to bring to the table possible new operational and organizational models for Saint Louis University to look at and provide the users, team and leadership with sufficient information and time to make good decisions.
Not all new ideas are appropriate, but we wanted to make sure that ideas were explored and presented in a way that there could be careful evaluation and consideration of them."
Frank Zilm, Chester Dean Director of the Institute for Health and Wellness Design