Why is discrete event simulation used for ED decision making?

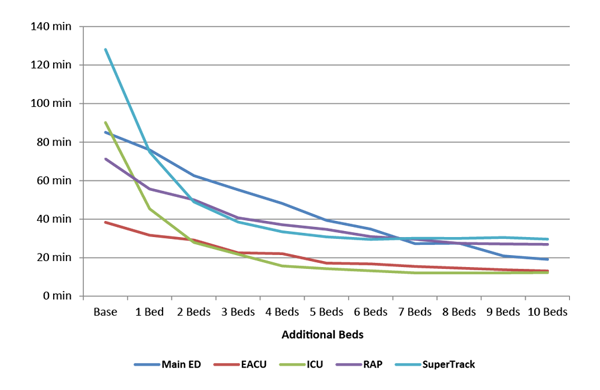
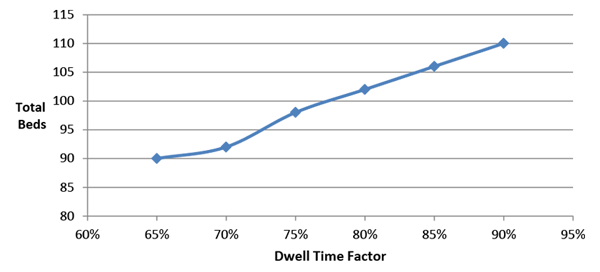
Discrete event simulation is a very powerful tool for decision making. By using simulation software like SIMUL8, hospitals are able to test ideas and assumptions for improvements.
This is very effective in settings such as the emergency department where there is a lot more variation and unpredictability, particularly in how patients arrive.
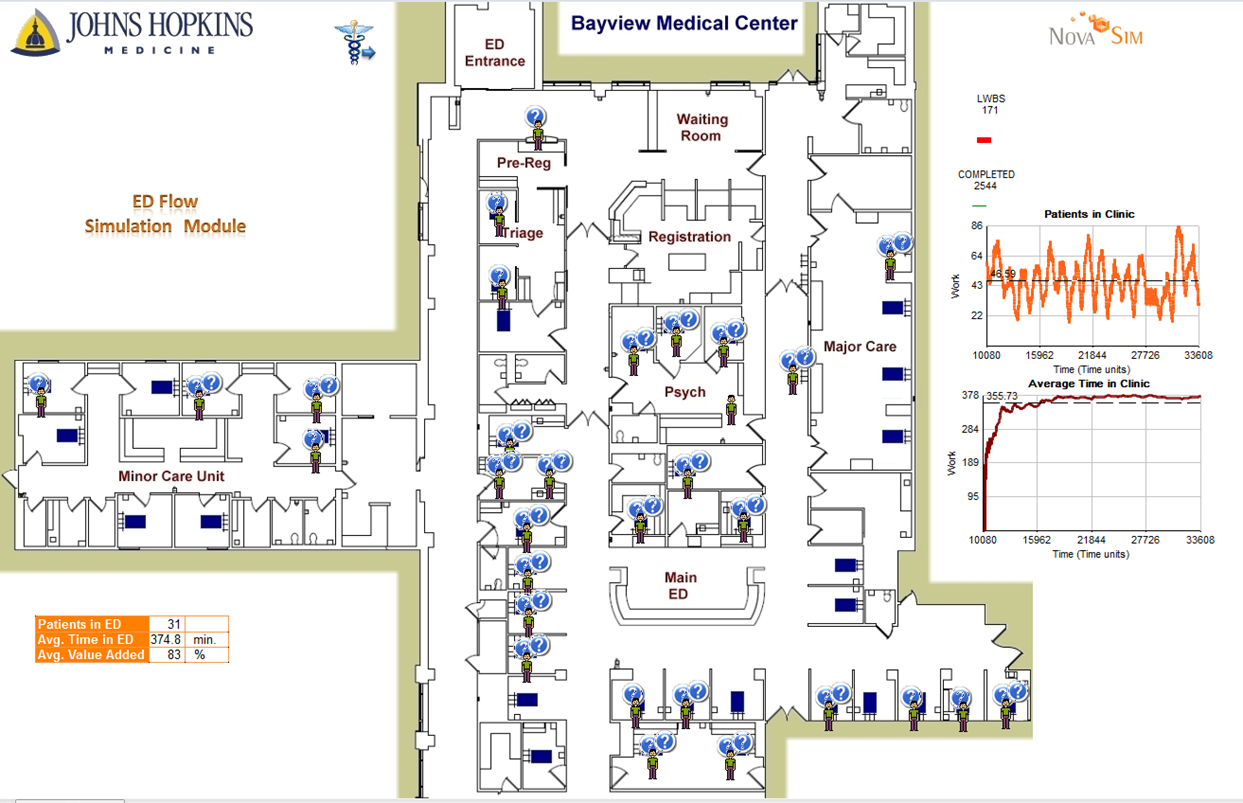
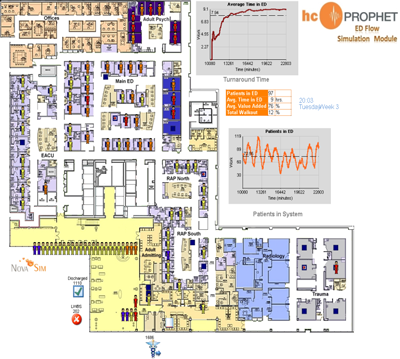
Over the last 10 years, Johns Hopkins Health System has relied on simulation to identify and implement a range of improvements to patient flow across their network of emergency department facilities; from its early use at Howard County Hospital through to its use at its largest trauma center at Johns Hopkins Hospital.
Learn more: Read Johns Hopkins Health System's Eric Hamrock's seven tips for using simulation in successful performance improvement programs.